Recent research has demonstrated the effectiveness of a novel therapy in reducing the size of challenging prostate and bladder cancers in mice. This therapy involves reprogramming immune cells to enhance their antitumor activity (1✔ ✔Trusted Source
Metabolic reprogramming of tumor-associated macrophages using glutamine antagonist JHU083 drives tumor immunity in myeloid-rich prostate and bladder cancer tumors
).
The research was conducted by the Johns Hopkins Kimmel Cancer Center, along with its Bloomberg~Kimmel Institute for Cancer Immunotherapy and Johns Hopkins Drug Discovery.
The research findings were published online on May 3 in the journal, Cancer Immunology Research, which is affiliated with the American Association for Cancer Research.
Advertisement
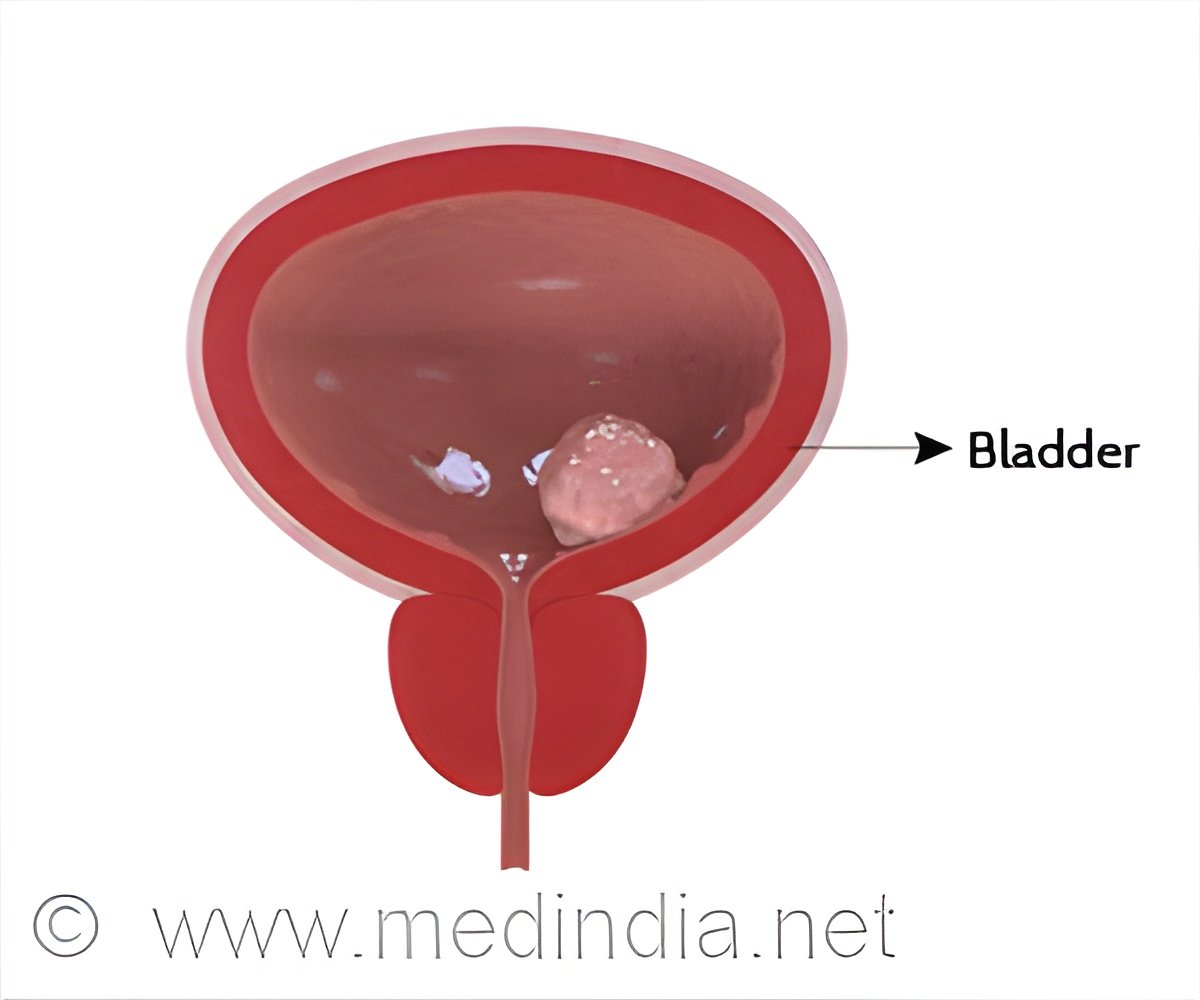
Immunotherapy in Cancer Treatment
Immunotherapies have revolutionized cancer care by enhancing the immune systems ability to detect and combat tumors. However, these treatments have not proven effective against aggressive prostate and bladder cancers. In an effort to improve the efficacy of immunotherapies in these types of cancer, researchers in the field of oncology, led by Jelani Zarif, Ph.D., the Robert E. Meyerhoff Endowed Professor and associate professor of oncology at Johns Hopkins, have been investigating the role of macrophages, a type of immune cell, in hindering the immune response to these cancers. They expressed that under certain conditions, macrophages promote tumor growth and suppress the activity of T-cells, which are responsible for killing tumor cells.
Zarif stated, “The focus of our work is to reprogram the immune-suppressive tumor-associated macrophages into anticancer immune cells to enhance therapeutic responses to immunotherapies and other standard-of-care cancer therapies,”.
The amino acid glutamine plays a crucial role in supporting the immune-suppressing macrophages. In a previous study, Zarif and his team showed that monocytes, which are precursor cells of macrophages, can transform into immune-activating macrophages when cultured in a glutamine-free laboratory environment. However, when monocytes are cultured with glutamine, they differentiate into immune-suppressing macrophages.
Advertisement
Blocking access to Glutamine converts macrophages to immune-stimulating type
Zarif and his colleagues postulated that by obstructing the immune cells’ access to glutamine, certain medications could alter the composition of macrophages in favor of the immune-stimulating variety, thereby aiding in tumor reduction. Research has demonstrated that a compound known as 6-diazo-5-oxo-L-norleucine (DON), which deprives tumors of glutamine, effectively diminishes the size of glutamine-dependent tumors. However, the advancement of DON as a cancer therapy was discontinued many years ago due to its detrimental impact on the gastrointestinal system and its side effects.
Advertisement
Experimental Glutamine-blocking Drug
Zarif opted for an experimental glutamine-blocking drug, JHU083, developed by study co-authors Barbara Slusher, Ph.D., director of Johns Hopkins Drug Discovery, and Jonathan Powell, M.D., Ph.D., former associate director of the Bloomberg~Kimmel Institute for Cancer Immunotherapy. The drug is a prodrug that transforms into an active drug within the tumor, minimizing adverse effects in other parts of the body. Research indicates that JHU083 effectively reduces tumor size, inhibits cancer metastasis, and enhances survival rates in animals with various types of cancer.
Zarif explained, “Barbara Slusher and her team changed the drug’s chemistry so it can circulate inactive throughout the body, and it only becomes active when it gets inside cancer cells,”.
Zarif further added. “Because the active form is only released to cancer cells, you can give a lower dose, further reducing the risk of side effects.”
Zarif and his colleagues demonstrated that JHU083 inhibits glutamine utilization in prostate and bladder tumors in mice, reducing tumor growth and inducing cell death. JHU083 also reprograms immune-suppressing macrophages into immune-boosting macrophages, which help destroy tumor cells and help add tumor-killing T-cells and natural killer cells to the tumors. However, adding a checkpoint inhibitor, an immunotherapy agent did not enhance JHU083’s effects, possibly due to the already strong antitumor immune activity in JHU083-treated tumors.
“JHU083 could be a promising anti-cancer therapy for tumors with immune-suppressing macrophages and too few T-cells,” he says. “It might also be a promising agent for tumors that do not respond to checkpoint inhibitors.”
Zarif intends to initiate a clinical trial for JHU083 in patients suffering from prostate or bladder cancer that is resistant to treatment, to assess if it has the potential in reducing tumor size and preventing metastasis. Zarif intends to collaborate with his colleagues at Johns Hopkins University to conduct this trial.
Together, they also aim to further review if the efficacy of JHU083 against tumors can be improved by combining with other treatments.
In summary, this groundbreaking research offers new hope for treating challenging prostate and bladder cancers by harnessing the power of reprogrammed immune cells.
Reference:
- Metabolic reprogramming of tumor-associated macrophages using glutamine antagonist JHU083 drives tumor immunity in myeloid-rich prostate and bladder cancer tumors – (https://aacrjournals.org/cancerimmunolres/article/doi/10.1158/2326-6066.CIR-23-1105/745149/Metabolic-reprogramming-of-tumor-associated)
Source-Medindia