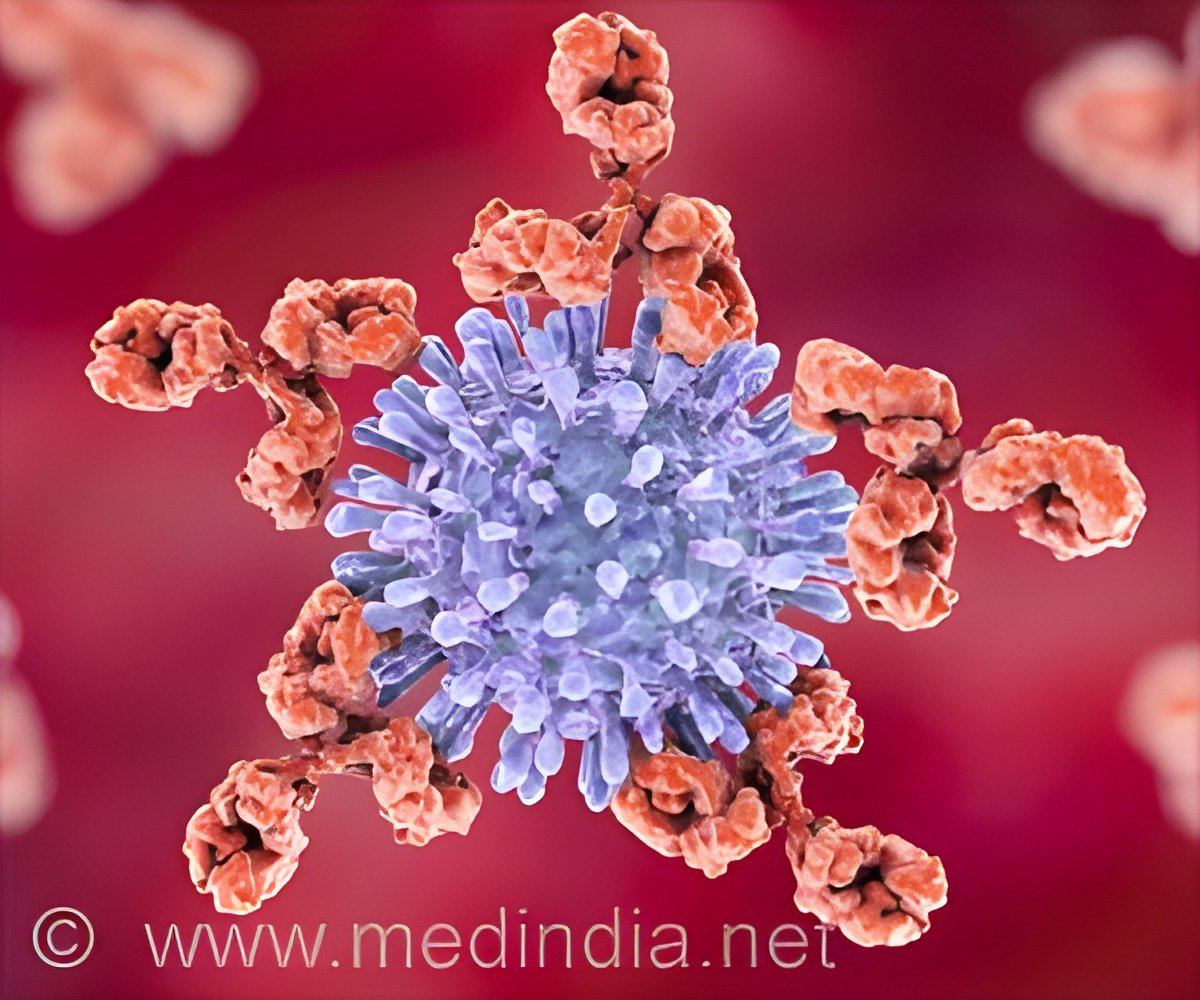
Cardiovascular disease represents the primary cause of mortality among individuals diagnosed with lupus, an autoimmune disorder. Lupus is characterized by the immune system’s attack on the body’s own tissues and organs, including the heart, blood vessels, lungs, joints, brain, and skin. Lupus myocarditis, which refers to the inflammation of the heart muscle, poses significant risks as it disrupts the normal rhythm and strength of the heartbeat. However, the underlying mechanisms of this intricate disease remain inadequately understood and challenging to investigate (1✔ ✔Trusted Source
An engineered human cardiac tissue model reveals contributions of systemic lupus erythematosus autoantibodies to myocardial injury
).
There is always a question regarding lupus, why some patients experience myocarditis while others do not. In addition, why the clinical symptoms among those affected vary significantly, ranging from asymptomatic conditions to severe heart failure. Lupus is distinguished by the presence of several autoantibodies, which are immune proteins that erroneously attack the body’s own tissues or organs, showing diverse specificities for various molecules. Similar to genetic factors, these autoantibodies may clarify the reasons why symptoms vary in different individuals.
Scientists have been long pursuing a theory that specific autoantibody profiles may provide insights into the unknown clinical differences seen in patients with lupus. To date, the identification of autoantibodies associated with cardiac damage has been difficult, primarily due to the absence of experimental models that accurately mimic cardiac disease in lupus patients. Existing animal models are inadequate due to variations in cardiac physiology, and human cell cultures fail to adequately represent the intricacies and functionality of the human heart.
How Autoantibodies Attack the Heart in Lupus Patients
In a recent study, scientists have reported autoantibodies independently influence heart function in patients with lupus. This study was published by scientists from Columbia Engineering, Columbia University Vagelos College of Physicians and Surgeons, and Harvard University on August 15 in Nature Cardiovascular Research.
The researchers engineered millimeter-sized cardiac tissues from healthy adult human stem cells, matured them using metabolic and electromechanical signals, and then incubated them with the autoantibodies found in the blood of lupus patients with and without myocarditis. The team found that the binding patterns of the patients’ autoantibodies to heart tissue depend on the type and severity of their myocardial damage. A subset of patients with severe myocarditis had unique autoantibody populations that primarily targeted dying cardiac cells, whereas patients with weakened heart pump function had autoantibodies that mostly targeted the surface of live cells. Interestingly, the team discovered that the autoantibodies that were binding to live cardiac cells were able to exert potent biological effects on the tissues in the absence of immune cells, revealing potentially new mechanisms that could contribute to heart failure in lupus patients.
The study also identified four such autoantibodies that may directly affect the heart muscle. These findings may help identify lupus patients with the greatest risk of developing heart disease, inform the development of new therapeutic strategies, and allow extension to other autoimmune diseases.
“This finding is the first demonstration that autoantibodies can directly mediate myocardial injury in this complex autoimmune disease,” said the team’s leader Gordana Vunjak-Novakovic, University Professor and the Mikati Foundation Professor of Biomedical Engineering, Medical Sciences, and Dental Medicine at Columbia. “It’s astounding that these tiny heart tissues we’ve engineered using human stem cells and ‘organs-on-chip’ technology have the ability to emulate organ-level functions in a patient-specific way, and for such a complex disease. We now live in the era of studying the progression and treatment of diseases using apparently simple yet highly controllable and predictive models of human organs. It feels like living in the future.”
Advertisement
Teams Collaborate to Develop Human Heart Model to Assess Effect of Autoantibodies on Heart Function
Vunjak-Novakovic, a bioengineer renowned for her pioneering work in engineering functional human tissue for use in regenerative medicine, and her group have spent three decades working on modeling heart injury and disease and engineering tissues to combat them. For this study, the bioengineers teamed up with two physicians, Robert Winchester and Laura Geraldino-Pardilla, both rheumatologists at New York-Presbyterian/Columbia University Irving Medical Center. The physicians provided blood samples containing lupus autoantibodies and detailed clinical data for the cohort of lupus patients. This enabled the Columbia Engineering team to assess the effects of patient-specific autoantibodies on heart function using engineered heart tissues and to correlate these effects to clinical symptoms.
“Myocarditis can be a diagnostically elusive and sometimes clinically ominous feature of lupus. The development of this functional mature cardiac tissue model is already opening multiple new pathways to advance our understanding and ultimately clinical management of this enigmatic autoimmune process,” Winchester noted.
Advertisement
To learn more about the potential therapeutic targets, Vunjak-Novakovic’s team also worked closely with Drs. Christine and Jonathan Seidman from Harvard University. The team is now exploring ways to use their findings to better understand the underlying mechanisms of cardiac disease in lupus patients and to improve diagnostics and treatment of this complex and challenging disease.
“What’s really cool about this study is that by leveraging our expertise in engineering and stem cells to develop models of the human heart, we were able to take an innovative approach to solving long-standing questions surrounding heart disease in lupus patients,” said the study’s first author Sharon Fleischer, who is a postdoc in Vunjak-Novakovic’s lab. “The new framework we established in this study to investigate autoantibody interactions with human organs opens up unparalleled opportunities for understanding organ damage, not just in lupus but across a spectrum of autoimmune diseases.”
“It was wonderful to be part of such a collaborative team that included engineers, physicians, and biologists working together to investigate a challenging clinical problem,” said Trevor Nash, one of the study’s co-first authors who is a recent graduate from the Vunjak-Novakovic lab and a MD/Ph.D. candidate in the Medical Scientist Training Program at the Vagelos College of Physicians and Surgeons.
Reference:
- An engineered human cardiac tissue model reveals contributions of systemic lupus erythematosus autoantibodies to myocardial injury
– (https://www.nature.com/articles/s44161-024-00525-w)
Source-Eurekalert