Microchips with brain and lung tissue can help in understanding and treating neurological symptoms, such as brain fog, associated with respiratory diseases like influenza.
The Biomedical Advanced Research and Development Authority (BARDA), part of the Administration for Strategic Preparedness and Response (ASPR) within the US Department of Health and Human Services (HHS), awarded a three-year contract to researchers at the University of Rochester to develop a technology to model respiratory disease effects on the brain and test therapeutic drugs to prevent and treat symptoms. The base-year is funded at $2.4 million with two option years which, if fully funded, would total $7.1 million.
Using Microphysiological Systems (MPS) to Tackle Neurological Symptoms
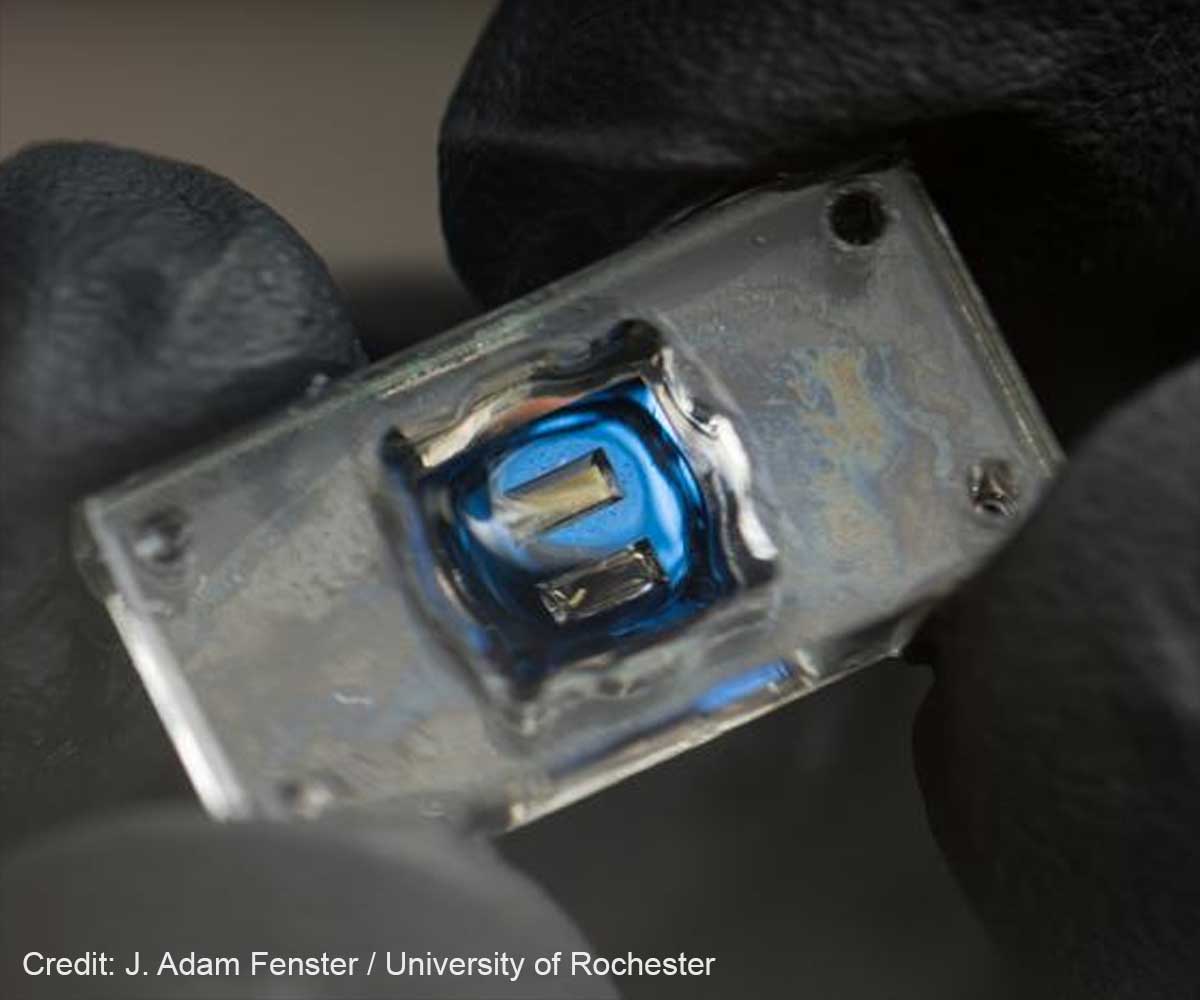
The project will use microphysiological systems (MPS)— small chips with ultrathin membranes supporting 3D networks of human cells, also known as “tissue chips” —to simulate infection and treatment in vitro. This tissue chips will incorporate human lung and brain tissue models.
“This is another step toward making disease modeling and drug discovery focused from the very beginning on more complex, human-relevant systems,” says principal investigator Benjamin Miller, a Dean’s Professor of Dermatology at Rochester with joint appointments in biomedical engineering, biochemistry and biophysics, optics, and materials science. “These chips can help make the whole drug discovery process faster.”
The project builds on work at Rochester’s recently established Translational Center for Barrier Microphysiological Systems (TraCe-bMPS) to build FDA-qualified drug development tools for studying the body’s barrier functions in combating disease. The center was created earlier this year with a $7.5 million grant from the National Institutes of Health (1✔ ✔Trusted Source
Researchers will use tissue-on-chip technology as a new way to explore the relationship between the lungs and brain
Co-investigator James McGrath, the William R. Kenan Jr. Professor of Biomedical Engineering and director of TraCe-bMPS, has been using microphysiological systems to study the mechanism by which inflammatory factors can enter the brain through the circulation and cause injury. The new BARDA-funded project will link two of McGrath’s modular, mass-producible chips specialized to mimic different organs.
“This project will connect this ‘brain’ chip upstream of a second chip that models a common source of those injurious factors: the infected lung,” says McGrath. “I’m thrilled to be working with a highly interdisciplinary Rochester team and with BARDA to develop what will be a scientifically important new tool.”
Advertisement
Lung-Brain Chip: Discovering the Connection
As with Long COVID, common viruses such as influenza can produce chronic symptoms such as brain fog, fatigue, and enduring pain. The project offers a new way to explore the relationship between the lungs and brain.
“The respiratory tract, with its cellular, humoral and hard-wired conduits to the brain, stands as the first line of defense against emerging infectious threats from zoonotic spillovers,” says co-investigator Harris “Handy” Gelbard, director of the Center for Neurotherapeutics Discovery at the University of Rochester Medical Center.
Advertisement
“We and our collaborators, with the support of the National Institute on Aging, have worked for the past several years to investigate these mechanisms in the hopes of applying therapeutic agents to ameliorate neurologic disease, especially in the elderly that are vulnerable to these infections. Now, with a world-class team of in-house experts at developing labs-on-a-chip, we have the unique opportunity to fast-track our research in a new lung-to-brain chip.”
David Dean, professor of pediatrics, biomedical engineering, and pharmacology and physiology, has studied the disease processes that lead to acute respiratory distress syndrome (ARDS) in the hopes of developing new treatments for this devastating disease.
“Studying this required us to use cultured cells from the lung, but almost always, these are grown and studied by themselves, which is not anywhere close to the situation in the lung where over 40 different cell types co-exist and interact to allow us to live. Thus, this is way too simplistic of a model,” says Dean, co-investigator of the project. “On the other extreme, we have used animal models to test hypotheses and drugs in development, but these models are so hard to control and make sense of because so many different things are going on, and it is difficult to attribute a response to a single pathway, leading to a system that is almost too complicated.”
He says the new approach is a win-win solution that will allow the researchers to mimic complex interactions between key cell types in the lung but in a controlled manner.
David Topham, the Marie Curran Wilson and Joseph Chamberlain Wilson Professor of microbiology and immunology and director of the Translational Immunology and Infectious Diseases Institute will also serve as a co-investigator and Hani Awad, the Donald and Mary Clark Distinguished Professor in Orthopaedics and a professor of biomedical engineering, will act as a consultant. The team will be working with University of Rochester spinout companies Phlotonics to do medium-throughput instrumentation and SIMPore to develop the chips.
The project will last three years, and by the end of the first year, the team aims to link the tissue chip systems with immune cells, demonstrate that they can infect the lung chip with influenza, and observe an inflammatory response in the brain chip.
References:
- Researchers will use tissue-on-chip technology as a new way to explore the relationship between the lungs and brain – (https://www.rochester.edu/newscenter/lung-to-brain-microchips-viral-neuroinflammation-622662/)
Source-Eurekalert