They also evolve, learning to produce more powerful “memory antibodies” that are better at neutralizing the virus and adapting to variants. Vaccination produces greater amounts of circulating antibodies than natural infection.
While vaccination gives rise to memory B cells that evolve over a few weeks, natural infection births memory B cells that continue to evolve over several months. “While a natural infection may induce maturation of antibodies with broader activity than a vaccine doesa natural infection can also kill you,” says Michel C. Nussenzweig, the Zanvil A. Cohn and Ralph M. Steinman Professor and head of Rockefeller’s Laboratory of Molecular Immunology. “A vaccine won’t do that and protects against the risk of serious illness or death from infection.”
When any virus enters the body, immune cells churn out hordes of circulating antibodies. These antibodies may protect us for months or years, but then dwindle in number, allowing reinfection. The immune system has a backup plan: an elite cadre of memory B cells.Until now, scientists didn’t know if the vaccines would produce the same type of robust memory B cell response as natural infection.
By comparing blood samples from convalescent COVID-19 patients to those from mRNA-vaccinated individuals who had never experienced natural infection, Nussenzweig and colleagues were able to tease out any differences in memory B cell evolution. The number of memory B cells produced by vaccination and natural infection was similar.
Between the first and second doses of the Pfizer and Moderna vaccines, memory B cells evolved quickly, producing increasingly potent memory antibodies. However, after two months, progress came to a halt. The memory B cells had been pre-programmed.
The memory B cells were present in large numbers and expressed potent antibodies, but the antibodies were not getting any stronger. Also, although some of these antibodies were able to neutralize Delta and other variants, there was no overall improvement in breadth. With convalescent patients, on the other hand, memory B cells continued to evolve and improve up to one year after infection. More potent and more broadly neutralizing memory antibodies were coming out with every memory B cell update.
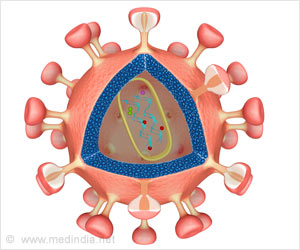
Memory B cells produced by a natural infection shall outperform those produced by mRNA vaccines for so many reasons, say researchers. Viruses that enter through the respiratory tract may have a different reaction in the body than viruses that are injected into our upper arms.
Perhaps an intact virus stimulates the immune system in a way that the vaccine’s lone spike protein simply cannot. Perhaps it’s because the virus lives for weeks in the naturally infected, giving the body more time to mount a strong defense. The vaccine, on the other hand, is quickly flushed out of the body after eliciting the desired immune response.
A booster with the currently available mRNA vaccine would engage memory cells to produce circulating antibodies that are strongly protective against the original virus and somewhat less so against variants.
“When to administer the booster depends on the object of boosting,” he says. “If the goal is to prevent infection, then boosting will need to be done after 6 to 18 months depending on the immune status of the individual. If the goal is to prevent serious disease, boosting may not be necessary for years.”
Source: Medindia