They found that at a total daily dose of 100 mg or more, milvexian resulted in better clot protection but no increase in bleeding compared with enoxaparin, the control drug. Milvexian was evaluated in daily doses ranging from 25 to 400 mg; there was no increase in bleeding over this wide range of doses.
“The major side effect of current oral anti-clotting drugs is bleeding, and the fear of bleeding leads to their underuse. This sets the need for safer oral anticoagulants and that is where milvexian comes in,” said senior author Jeffrey Weitz.
He is a professor of medicine and biochemistry and biomedical sciences at McMaster. He is also the executive director of the Thrombosis and Atherosclerosis Research Institute of McMaster and Hamilton Health Sciences.
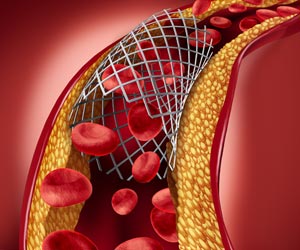
“Blood clots are responsible for 1 in 4 deaths worldwide. Anticoagulants (blood thinners) are a mainstay for the treatment and prevention of clots in veins and arteries and we urgently need safer oral medications to reduce the burden from what are often lifelong conditions.”
The study was published today in the New England Journal of Medicine and Weitz presented a summary of the findings at a late breaking session at the 2021 American Heart Association Scientific Sessions.
Weitz said that blood clots are the underlying cause of heart attack, stroke, deep vein thrombosis, and pulmonary embolism. Many of these conditions require lifelong anticoagulant treatment. Therefore, there is a need for safer oral anticoagulants like milvexian.
He said the study focused on patients undergoing knee replacement surgery because they are at high risk for postoperative blood clots and such clots can be readily identified with venograms, x-rays of the veins of the legs. Therefore, this patient population provides an ideal testing ground for new anticoagulants because effective and safe doses can be identified.
Weitz said his milvexian study is the first of several investigations of oral factor XIa inhibitors. The results of the other studies will likely be released next year.
Funding for the study was provided by the pharmaceutical firms Bristol Myers Squibb and Janssen Research and Development.
Source: Eurekalert