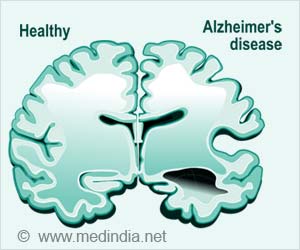
In previous research, researchers found that subtle brainwaves detectable with EEG are the strongest predictor of hidden consciousness and eventual recovery for unresponsive brain-injured patients. But the precise pathways in the brain that become disrupted in this condition were unknown.
In the new study published in the journal Brain, researchers used EEG to examine 107 brain injury patients. The technique can determine when patients are trying, though unable, to respond to a command such as “keep opening and closing your right hand”.
Finding the Source of Hidden Consciousness in ‘Comatose’ Brain Injury Patients
The analysis detected CMD in 21 of the patients. Later, they analyzed structural MRI scans from all the patients. Using a technique, they developed called bi-clustering analysis to identify patterns of brain injury that are shared among patients with CMD and contrast to those without CMD.
Advertisement
They found that all the CMD patients had intact brain structures related to arousal and command comprehension, supporting the notion that these patients were hearing and understanding the commands but were unable to carry them out.
All the CMD patients had deficits in brain regions responsible for integrating comprehended motor commands with motor output, preventing CMD patients from acting on verbal commands.
The findings could help physicians more quickly identify brain-injured patients who might have hidden consciousness and better predict which patients are likely to recover with rehabilitation().
More research is required before these approaches can be applied to clinical practice. However, the study shows that it may be possible to screen for hidden consciousness using widely available structural brain imaging, moving the detection of CMD one step closer to general clinical use.
Not every critical care unit may have resources and staff that is trained in using EEG to detect hidden consciousness, so MRI may offer a simple way to identify patients who require further screening and diagnosis.
References:
- Schiff, Nicholas D. Cognitive Motor Dissociation Following Severe Brain Injuries. JAMA neurology vol. 72,12 (2015): 1413-5.(https://jamanetwork.com/journals/jamaneurology/article-abstract/2456130)
- Jöhr, Jane et al. Recovery in cognitive motor dissociation after severe brain injury: A cohort study.” PloS one vol. 15,2 e0228474. 5 Feb. 2020.(https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0228474)
Source: Eurekalert