Advanced imaging reveals hidden metastases in high-risk prostate cancer cases, offering new insights for better diagnosis and treatment strategies.

Many cases of high-risk nonmetastatic hormone-sensitive prostate cancer may be more advanced than previously believed, revealed a recent study.
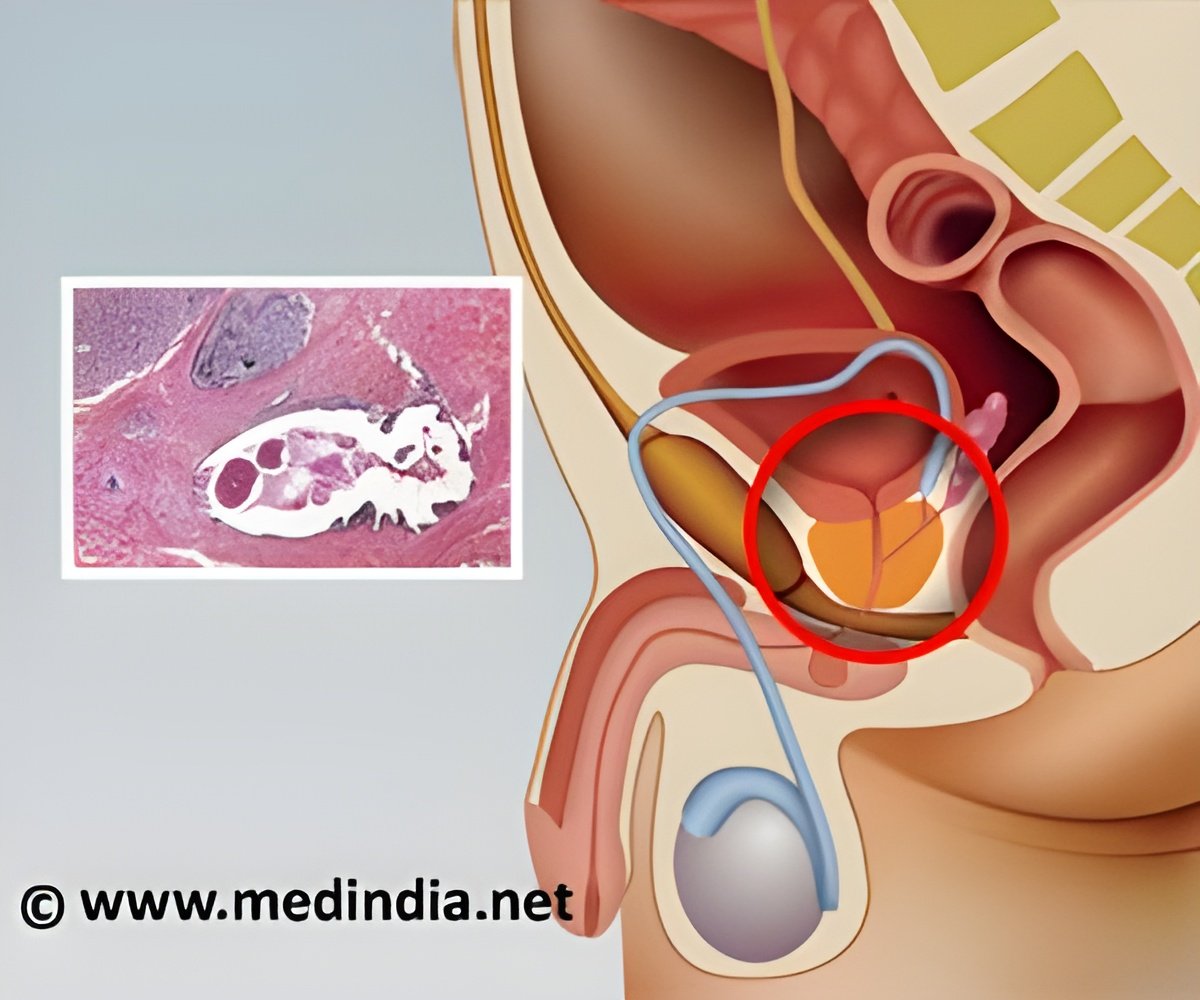
The study, published in JAMA Network Open, found that nearly half of high-risk prostate cancer patients previously classified as nonmetastatic by conventional imaging actually have metastatic disease when evaluated with advanced prostate-specific membrane antigen–positron emission tomography (PSMA-PET) imaging, suggesting that traditional imaging may underestimate how far the cancer has spread in many cases.
The PSMA-PET Revolution in Prostate Cancer
This advanced imaging technology plays a critical role in redefining how prostate cancer is staged. PSMA-PET imaging uses tiny amounts of radioactive “tracers,” called radiotracers, that binds to prostate cancer cells, making them visible on PET scans. Unlike conventional imaging, which provides only anatomical details, PSMA-PET offers functional imaging that reveals the cancer’s biological activity, which can significantly improve the accuracy of disease staging.
The clinical adoption of PSMA-PET has changed the landscape of prostate cancer imaging, yet treatment decisions often rely on clinical trials that did not incorporate this advanced imaging technique for patient selection.
To better understand the advantages of PSMA-PET over conventional imaging, researchers conducted a post hoc, retrospective cross-sectional study using data from 182 patients with high-risk recurrent prostate cancers who were thought to have disease limited to the prostate and were eligible for the EMBARK trial.
This clinical trial previously demonstrated that adding enzalutamide, a type of hormone therapy, to androgen deprivation therapy significantly improves metastasis-free survival. However, the trial relied on conventional imaging to classify patients, which researchers believe might have underestimated the disease’s extent in some cases.
In the cohort of patients, the researchers found PSMA-PET detected cancer metastases in 46% of patients, even though traditional imaging had suggested no evidence of cancer spread.
Advertisement
“We anticipated that PSMA-PET would detect more suspicious findings compared to conventional imaging. However, it was informative to uncover such a high number of metastatic findings in a well-defined cohort of patients resembling the EMBARK trial population that was supposed to only include those without metastases,” said Dr. Adrien Holzgreve, a visiting assistant professor at the David Geffen School of Medicine and first author of the study.
These results challenge the interpretation of previous studies, like the EMBARK trial, and support the inclusion of PSMA-PET for patient selection in clinical and trial interventions in prostate cancer in future major industry-sponsored clinical trials. It also highlights the need to reevaluate treatment strategies and opens the door to potentially curative options for some patients, such as targeted radiotherapy, while raising important questions about integrating new imaging technologies into standard care.
Advertisement
While the current findings underscore PSMA-PET’s potential, researchers are continuing to explore its broader applications through additional studies. More research is needed to understand its impact on long-term patient outcomes and how it can best guide therapy, noted Calais.
“We have good rationales to assume that it is helpful to primarily rely on PSMA-PET findings,” said Holzgreve. “But more high-quality prospective data would be needed to claim superiority of PSMA-PET for treatment-guidance in terms of patient outcome. However, we are confident PSMA-PET will continue to advance prostate cancer staging and guide personalized therapies.”
Ongoing efforts at UCLA include analyzing follow-up data from four UCLA trials to assess how PSMA-PET findings influenced treatment decisions and patient outcomes. Additionally, as part of an international consortium studying over 6,000 patients, the team is investigating the prognostic value of PSMA-PET.
Source-Eurekalert