Researchers stress that HPAI H5N1 must be closely monitored for genetic changes, especially as cases rise in humans exposed to infected birds, cows, or mammals.

The highly pathogenic avian influenza (HPAI) H5N1 influenza virus that is presently circulating in dairy cows in the United States could be more easily spread to humans because of a single mutation in a protein on its surface.
The study was published in the journal Science (1✔ ✔Trusted Source
A single mutation in bovine influenza H5N1 hemagglutinin switches specificity to human receptors
). According to the study’s findings, HPAI H5N1 has to be continuously and closely watched for any genetic alterations that can increase the virus’s ability to infect humans.
People who have been exposed to infected wild birds, poultry, dairy cows, and other mammals have contracted the bovine (cow) H5N1 virus, however, current strains are not known to be communicable.
Role of Hemagglutinin in H5N1 Infection
The H5N1 virus has been studied for years to learn about natural viral genetic alterations and their potential effects on transmissibility as part of pandemic preparedness measures.
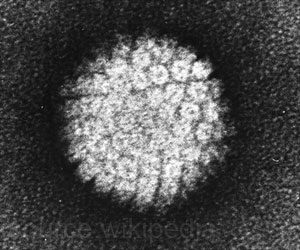
A surface viral protein known as hemagglutinin (HA) helps influenza viruses attach to cells. To spread infection, the HA binds to cell receptors for sugar (glycan) molecules.
Since the human upper respiratory tract lacks the avian-type cell receptors present in birds, avian (bird) influenza viruses, such as H5N1, have not frequently infected humans.
Researchers fear viruses may develop the ability to identify human-type cell receptors in the upper airways, allowing them to infect humans and spread from one person to another.
Advertisement
Role of HA Mutations in H5N1 Infectivity
Scientists at Scripps Research used the H5N1 strain isolated from the first U.S. human infection with the bovine strain 2.3.4.4b (A/Texas/37/2024) to test how mutations in the HA gene sequence affected the binding of that protein with avian versus human-type cell receptors.
The researchers introduced several mutations into the viral HA protein that had been observed to occur naturally in the past and found that one mutation, called Q226L, improved the ability of the protein to attach to receptors typically found on human cells, especially when an additional mutation was present.
Advertisement
Importantly, the researchers introduced the genetic mutations only into the HA surface protein and did not create or conduct experiments with a whole, infectious virus.
The experimental finding with the Q226L mutation alone does not mean HPAI H5N1 is on the verge of causing a widespread pandemic, the authors note. Other genetic mutations would likely be required for the virus to be transmitted among people.
In the setting of a growing number of H5N1 human cases resulting from direct contact with infected animals, the findings stress the importance of continued efforts at outbreak control and continued genomic surveillance to monitor for the emergence of HPAI H5N1 genetic changes and maintain public health preparedness.
Reference:
- A single mutation in bovine influenza H5N1 hemagglutinin switches specificity to human receptors- (https:www.science.org/doi/10.1126/science.adt0180)
Source-Eurekalert