The term “long COVID” refers to a range of persistent symptoms that can emerge or persist after the acute phase of the illness. Patients may continue to experience significant challenges long after their respiratory symptoms have improved, especially in terms of their neurological well-being.
Following this, a significant percentage of COVID-19 survivors, even those with mild cases, may experience cognitive decline and difficulty sustaining focus for extended periods. Therefore, it is crucial to explore how the illness affects the brain during the acute phase, as this could provide insights into these long-lasting neurological effects.
A recent study conducted at the D’Or Institute for Research and Education (IDOR) and published in the journal Brain, Behavior, & Immunity – Health, has identified molecular alterations that could potentially be responsible for the neurological symptoms observed in some patients. This emphasizes the importance of gaining a deeper understanding of these potential COVID-19 side effects.
COVID-19 continues to be a concerning disease even after the end of its pandemic phase. In the first half of 2024 alone, it was responsible for over 3,000 deaths in Brazil. Additionally, scientific literature has been extensively documenting the deleterious effects of the infection even after patients have recovered, a condition now known as “long COVID.”
Advertisement
Neurological Symptoms of Long COVID
The most common neurological symptoms are headaches, fatigue, loss of smell, and even more severe complications such as strokes and encephalitis. Investigating these manifestations is crucial, as we still know little about the mechanisms leading to these complications and how they develop(1✔ ✔Trusted Source
Changes in neuroinflammatory biomarkers correlate with disease severity and neuroimaging alterations in patients with COVID-19 neurological complications
)
.
Seeking biomarkers that could provide clues about neuroinflammatory processes in COVID-19, IDOR researchers analyzed data from patients confirmed to have COVID-19 who were hospitalized in the Rede D’Or network between April and November 2020.
The sample included 35 patients aged between 26 and 87 years, divided between moderate and severe cases, all of whom presented significant neurological symptoms during the acute COVID-19 infection. The data were collected from medical records and included imaging exams (MRI and CT scans), blood tests, and cerebrospinal fluid (CSF) analysis—a fluid that surrounds the brain and spinal cord. Ten CSF samples from uninfected patients served as a control group.
Advertisement
Brain Inflammation in COVID-19 Patients
The analysis revealed that most patients had at least one comorbidity, with 65.7% having two or more. About 85.7% of patients exhibited neurological symptoms at the time of hospital admission, a clinical picture that was even more pronounced than respiratory symptoms.
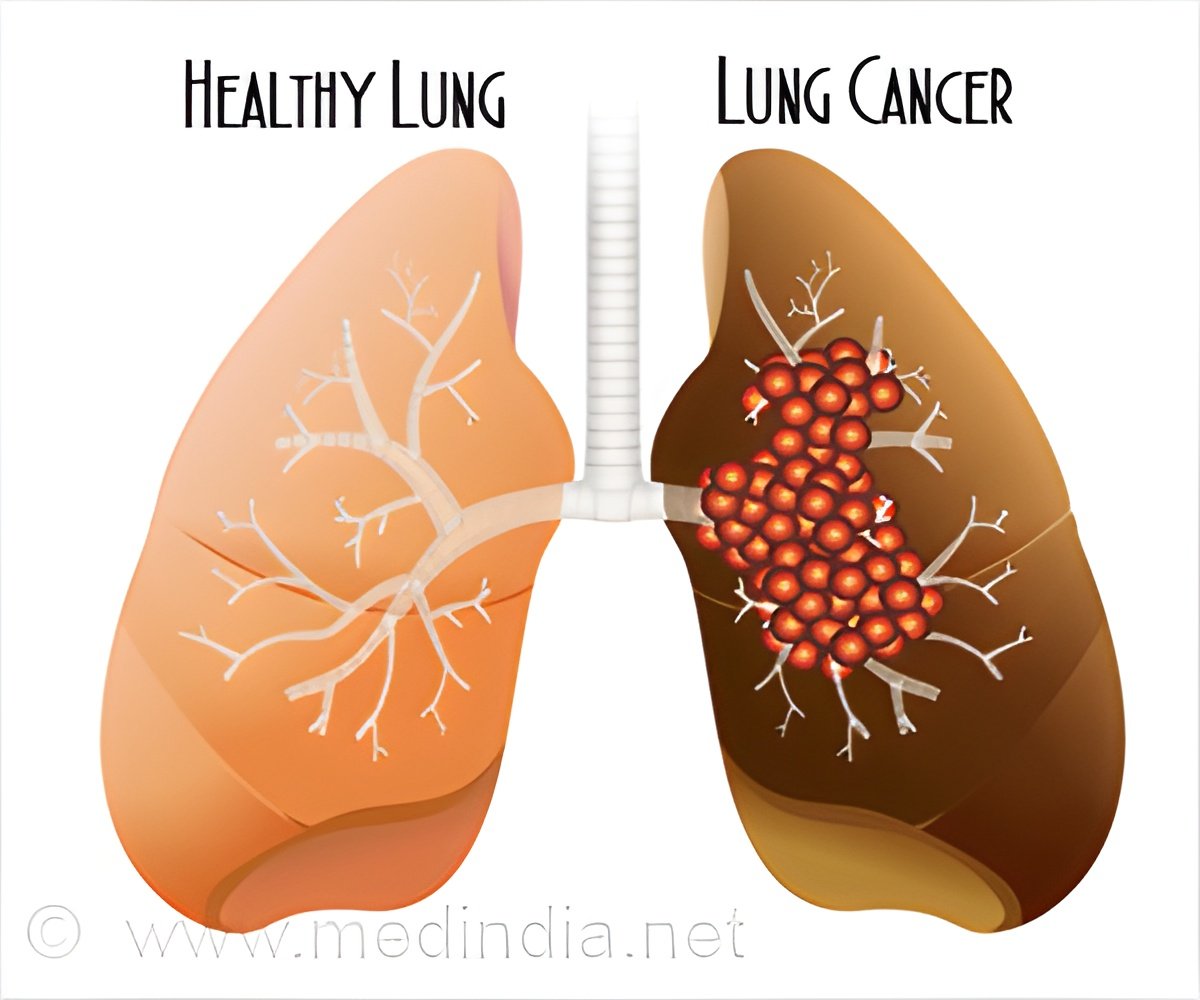
Imaging exams showed that 28.6% of patients had focal or diffuse brain changes associated with COVID-19, including demyelinating lesions, encephalitis, and stroke.
Blood tests indicated that 66% of patients showed signs of an exacerbated inflammatory response. Proteomic analyses of the CSF revealed an altered protein pattern compared to the controls, with 116 significantly dysregulated proteins related to the immune system and metabolic processes.
Advertisement
Neuroinflammatory Biomarkers and Disease Severity
The levels of two pro-inflammatory cytokines, interleukin-6 (IL-6) and tumor necrosis factor-α (TNFα), were elevated in the CSF of COVID-19 patients, with IL-6 being particularly higher in severe cases. These cytokines are associated with the severity of the disease and the changes observed in imaging exams.
Dr. Fernanda Aragão, a postdoctoral researcher at IDOR and the study’s first author, comments that the research is one of the first to connect imaging exams and neurological symptoms with neuroinflammatory biomarkers capable of reflecting the severity of acute disease, a complication that remains difficult to predict.
Despite the severity distinction found in these biomarkers, the researcher emphasizes that neuroinflammation is independent of disease severity and may be one of the main causes of neurological disorders associated with COVID-19. She points out that even patients with milder cases showed significant changes in the CSF, suggesting that the body’s inflammatory response may affect the brain in ways not yet fully understood.
“This study reveals that neuroinflammation is a common factor in neurological cases of the disease, even in patients with diverse conditions, whether moderate or severe. Identifying these inflammatory markers that connect COVID-19 severity and neuroimaging changes could be very important for developing therapies aimed at both treating acute COVID-19 infections and addressing the persistent effects of what is known as long COVID,” adds the author.
Long-Term Treatment and Monitoring
These findings highlight the need for long-term monitoring of patients who have had COVID-19, especially those at risk of developing persistent neurological complications. Better understanding of these mechanisms can help develop more effective treatment and prevention strategies in the future.
IDOR’s research provides valuable insights into the neurological impacts of COVID-19 and paves the way for future studies to explore these findings more deeply and in larger populations.
Thus, continued investigation into the neurological consequences of COVID-19 is presented as a crucial investment, especially with the evolution of new variants and the implementation of vaccination programs, to ensure that the long-term effects of the pandemic are adequately understood and addressed.
Reference:
- Changes in neuroinflammatory biomarkers correlate with disease severity and neuroimaging alterations in patients with COVID-19 neurological complications – ( https:doi.org/10.1016/j.bbih.2024.100805)
Source-Eurekalert