“These viral pandemic-associated signatures tell us how a person’s immune system responds to a viral infection and how severe it might get, and that gives us a map for this and future pandemics,” said Pradipta Ghosh, MD, professor of cellular and molecular medicine at UC San Diego School of Medicine and Moores Cancer Center.
‘Artificial Intelligence predicts how patients with viral infections, including COVID-19, will fare. Gene expression patterns associated with pandemic viral infections provide a map to help define patients’ immune responses, measure disease severity, predict outcomes and test therapies — for current and future pandemics.’
Ghosh co-led the study with Debashis Sahoo, PhD, assistant professor of pediatrics at UC San Diego School of Medicine and of computer science and engineering at Jacobs School of Engineering, and Soumita Das, PhD, associate professor of pathology at UC San Diego School of Medicine.
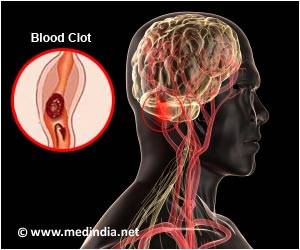
During a viral infection, the immune system releases small proteins called cytokines into the blood. These proteins guide immune cells to the site of infection to help get rid of the infection. Sometimes, though, the body releases too many cytokines, creating a runaway immune system that attacks its own healthy tissue. This mishap, known as a cytokine storm, is believed to be one of the reasons some virally infected patients, including some with the common flu, succumb to the infection while others do not.
But the nature, extent and source of fatal cytokine storms, who is at greatest risk and how it might best be treated have long been unclear.
“When the COVID-19 pandemic began, I wanted to use my computer science background to find something that all viral pandemics have in common — some universal truth we could use as a guide as we try to make sense of a novel virus,” Sahoo said. “This coronavirus may be new to us, but there are only so many ways our bodies can respond to an infection.”
The data used to test and train the algorithm came from publicly available sources of patient gene expression data — all the RNA transcribed from patients’ genes and detected in tissue or blood samples. Each time a new set of data from patients with COVID-19 became available, the team tested it in their model. They saw the same signature gene expression patterns every time.
“In other words, this was what we call a prospective study, in which participants were enrolled into the study as they developed the disease and we used the gene signatures we found to navigate the uncharted territory of a completely new disease,” Sahoo said.
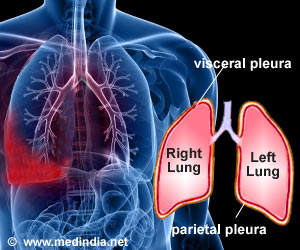
By examining the source and function of those genes in the first signature gene set, the study also revealed the source of cytokine storms: the cells lining lung airways and white blood cells known as macrophages and T cells. In addition, the results illuminated the consequences of the storm: damage to those same lung airway cells and natural killer cells, a specialized immune cell that kills virus-infected cells.
“We could see and show the world that the alveolar cells in our lungs that are normally designed to allow gas exchange and oxygenation of our blood, are one of the major sources of the cytokine storm, and hence, serve as the eye of the cytokine storm,” Das said. “Next, our HUMANOID Center team is modeling human lungs in the context of COVID-19 infection in order to examine both acute and post-COVID-19 effects.”
The researchers think the information might also help guide treatment approaches for patients experiencing a cytokine storm by providing cellular targets and benchmarks to measure improvement.
To test their theory, the team pre-treated rodents with either a precursor version of Molnupiravir, a drug currently being tested in clinical trials for the treatment of COVID-19 patients, or SARS-CoV-2-neutralizing antibodies. After exposure to SARS-CoV-2, the lung cells of control-treated rodents showed the pandemic-associated 166- and 20-gene expression signatures. The treated rodents did not, suggesting that the treatments were effective in blunting cytokine storm.
“It is not a matter of if, but when the next pandemic will emerge,” said Ghosh, who is also director of the Institute for Network Medicine and executive director of the HUMANOID Center of Research Excellence at UC San Diego School of Medicine. “We are building tools that are relevant not just for today’s pandemic, but for the next one around the corner.”
Source: Medindia