Researchers from the Stanford University in the US showed that in such people, the immune cells are better equipped to mobilize quickly against SARS-CoV-2, the virus responsible for Covid-19.
‘Memory cells are the most active in infectious-disease defense. They’re what you want to have in order to fight off a recurring pathogen.’
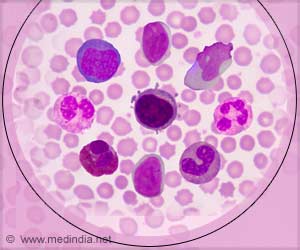
The immune cells, called killer T-cells, roam through the blood and lymph, park in tissues and carry out stop-and-frisk operations on resident cells.
The study, published in the journal Science Immunology, showed that killer T-cells taken from the sickest Covid-19 patients exhibit fewer signs of having had previous run-ins with common-cold-causing coronaviruses.
Many of these killer T cells were in “memory” mode, said Mark Davis, Professor of microbiology and immunology at the Stanford’s School of Medicine.
“Memory cells are by far the most active in infectious-disease defense. They’re what you want to have in order to fight off a recurring pathogen. They’re what vaccines are meant to generate,” Davis said.
For the study, the team analyzed blood samples taken from healthy donors before the Covid-19 pandemic began, meaning they’d never encountered SARS-CoV-2 — although many presumably had been exposed to common-cold-causing coronavirus strains.
They found that Covid-19 patients with milder symptoms tended to have lots of killer-T memory cells directed at peptides SARS-CoV-2 shared with other coronavirus strains.
Sicker patients’ expanded killer T-cell counts were mainly among those T-cells typically targeting peptides unique to SARS-CoV-2 and, thus, probably had started from scratch in their response to the virus.
“It may be that patients with severe Covid-19 hadn’t been infected, at least not recently, by gentler coronavirus strains, so they didn’t retain effective memory killer T cells,” Davis said.
Source: IANS