Individuals with the neurodegenerative condition Spinal Muscular Atrophy (SMA) are at an increased risk of developing fatty liver disease. This suggests that SMA patients may encounter additional health challenges over time, raising significant concerns about their long-term care and health outcomes.
What is Spinal Muscular Atrophy (SMA)
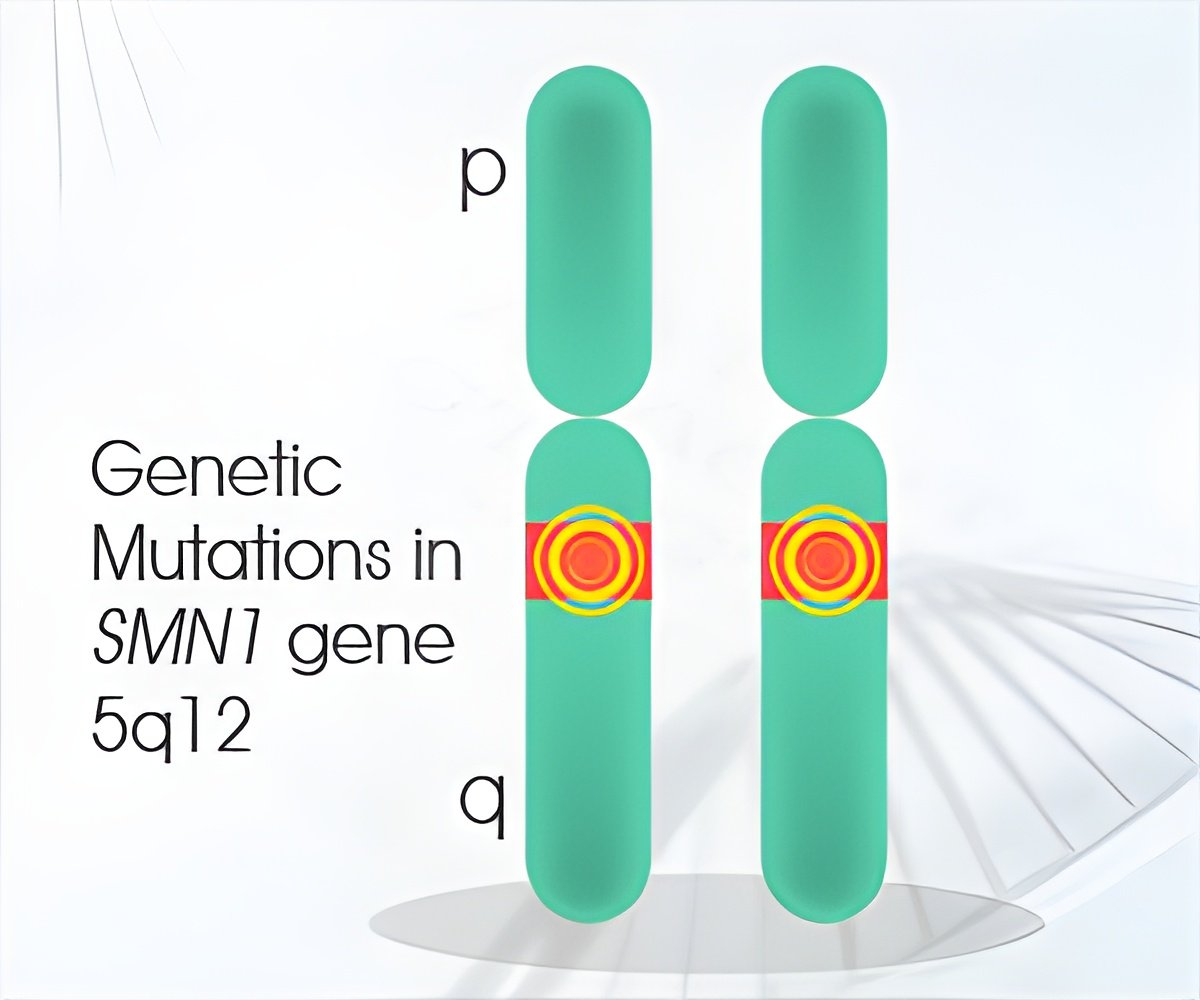
SMA is a rare genetic condition that prevents the body from producing Survival Motor Neuron (SMN), a protein essential for nerves that control movement. The damaged motor neurons are unable to send messages to the muscles, resulting in progressive muscle weakness. While recent advances in treatment have improved survival rates, particularly for babies with severe SMA, this new research indicates that the impact of SMA extends beyond the nervous system, potentially affecting other organs such as the liver.
Fatty liver disease, usually linked to heart conditions, diabetes, and obesity, is a condition in which fat builds up in the liver, causing inflammation and damage. The presence of fatty liver disease in mild and severe forms of SMA is particularly concerning, as it can have serious long-term consequences for the health of SMA patients in childhood and adulthood.
The multi-centre study, published in the prestigious Journal of Clinical Investigation, involved clinicians and researchers from leading institutions across Singapore, the United States, and Scotland, including the Agency for Science, Technology and Research (A*STAR), Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine),Boston Children’s Hospital, Harvard Medical School, Harvard University, and the University of Aberdeen.
The study revealed that the genetic mutation responsible for SMA reduces SMN protein levels in liver cells, impairing their ability to break down and use fat effectively. This finding explains the presence of fatty liver disease in SMA patients, which was detected in children as young as three years old through liver ultrasound scans. Crucially, editing the faulty gene in patients’ stem cells to increase SMN production reversed the liver dysfunction caused by the mutation, establishing a direct link between the genetic defect and liver problems in SMA.
“Our findings show that SMA patients may be at higher risk of additional health problems over time, as the SMA gene mutation also affects other organs in the body, including the liver,” said Dr Crystal Yeo, director of this research and Clinician-Scientist who directs the Translational Neuromuscular Medicine Laboratory at A*STAR’s Institute of Molecular and Cell Biology (IMCB). Dr Yeo is also a practicing Consultant Neurologist at National Neuroscience Institute (NNI).
“Since SMA patients are living longer, knowing that SMA affects other organs changes how doctors monitor and treat this condition,” says Prof Basil Darras, Chief of the Division of Clinical Neurology and Director of the Neuromuscular Center and SMA program from Boston Children’s Hospital and Harvard Medical School.
Advertisement
International collaborators Prof Simon Parson, Regius Chair of Anatomy from the University of Aberdeen, Prof Lee Rubin, co-Director of the Harvard Nervous System Diseases Program at Harvard University, and Prof Ong Wei Yi, Professor of Anatomy at NUS Medicine and NUS Life Sciences Institute, agree that while we now have life enhancing therapies for those affected by SMA, it is key that we understand which illnesses might affect these patients in future.
As individuals with SMA live longer due to improved treatment options, understanding the long-term effects of the genetic mutation on various organs becomes crucial for screening for previously unknown problems, developing effective treatment strategies and improving patient outcomes, such as survival and quality of life. Further research in this area could not only benefit those living with SMA but also provide insights into the treatment of other neurological conditions with similar disease mechanisms.
Advertisement