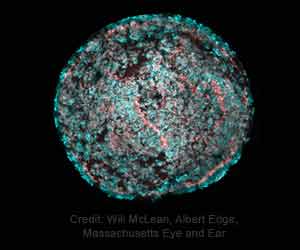
For sounds to be heard, sensory hair cells in the inner ear must make contact with the ear’s tectorial membrane, which vibrates in response to sound, and then convert these vibrations into signals sent to the brain.
The stereocilin protein acts as a scaffold, helping the hair cell microvilli stand up together in an organized bundle so that their tips can touch the membrane.
The technique could also be used in other situations where the therapeutic gene is very large, says Jeffrey Holt, Ph.D., a scientist in the departments of Otolaryngology and Neurology at Boston Children’s and the study’s senior investigator.
To deliver a healthy stereocilin gene, the team used a synthetic adeno-associated virus (AAV) that is effective in targeting hair cells.
The challenge faced was that the gene for stereocilin is too big to fit into the gene therapy vector. The gene is about 6,200 DNA base pairs long, but the AAV only has a capacity of 4,700 base pairs.
Researchers then came up with a solution to use an existing technique called protein recombination, where two halves of a protein find each other and hook up. But in this case, it didn’t work.
When they added the signal to both halves of the protein, the two halves successfully came together. They also found a robust restoration of full-length stereocilin protein in the mice and normal-appearing hair bundles that were able to contact the tectorial membrane.
They used two types of hearing tests: one similar to hearing tests used in babies, and a test using electrodes on the scalp to measure auditory brainstem responses to a range of sound frequencies and intensities.
On testing, the mice were found to be much more sensitive to subtle sounds and showed improved cochlear amplification, which is the ability to amplify soft sounds, tamp down the response to loud sounds, and discriminate among sounds of different frequencies more precisely.
In some mice, the hearing was restored to normal levels. Researchers have filed a patent application for the gene therapy technology.
According to Boston Children’s Hospital, approximately 100,000 patients in the U.S. and 2.3 million worldwide carry STRC mutations and they could potentially benefit from this therapy.
Researchers will now test whether the technique works with the human stereocilin gene and test it in human inner ear cells in a dish, derived from patients with STRC hearing loss. If gene therapy restores auditory function at the tissue level, they will apply to the FDA for permission to test it in humans.
Source: Medindia