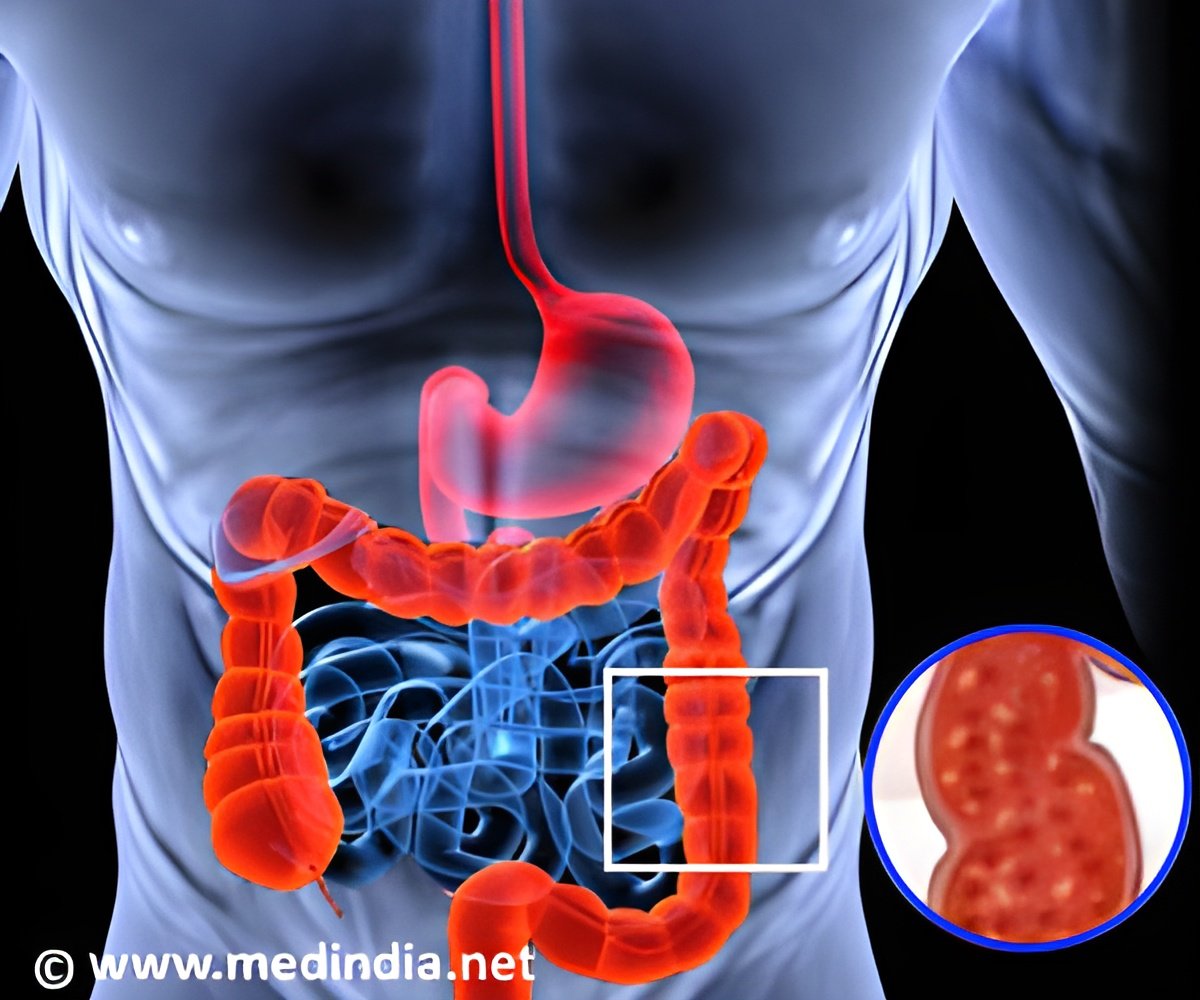
Ulcerative colitis (UC) is an inflammatory bowel illness that affects the lining of the large intestine, causing irritation, inflammation, and ulcers. Long-term UC is known to cause severe discomfort, diarrhea, stomach pain, food limitations, and weight loss, all of which affect a patient’s quality of life.
The cause of UC is not fully understood, but it is thought to involve a complex interaction of immune responses to gut microbes, intestinal abnormalities, and genetic and environmental factors.
Previous studies have found that when the intestinal tissue heals and inflammation is reduced, patients with ulcerative colitis UC can have better outcomes, spend less time in the hospital, and undergo fewer surgeries. However, even with these benefits, 30% of UC patients still experience tissue inflammation.
It is widely known that certain immune cell activation and intestinal disease activities are connected. Although their function in the digestive system is still unknown, they may be related to tissue healing.
To bridge this research gap, a team of researchers from China, led by Professor Zhanju Liu, sought to develop a diagnostic criterion based on changes in infiltrating immune cells in the large intestine, associated with tissue healing in patients with UC(1✔ ✔Trusted Source
Development and validation of a novel criterion of histologic healing in ulcerative colitis defined by inflammatory cell enumeration in lamina propria mucosae: A multicenter retrospective cohort in China
The Role of Immune Cell Activation in Ulcerative Colitis
Sharing his views on the importance of such an index, Prof. Liu elaborates, “Importantly, the assessment of activated immune cell infiltrations in the colonic lamina propria may provide a rationale for the precision diagnosis of histological healing in UC patients.” Their article was published in the Chinese Medical Journal.
The researchers analyzed the clinical, endoscopic, and tissue data of 220 patients with UC who underwent treatment and successfully achieved healing. The study was conducted between January 2017 and May 2022 across hospitals in China.
Advertisement
They analyzed the levels of the surface proteins CD177, CD64, CD40L, and CD69, which are the biomarkers of activated immune cells, namely neutrophils and T cells.
Further, they correlated the proportion of activated immune cells with six characteristic features of the colon namely
Advertisement
- acute inflammatory cell infiltration,
- crypt abscesses (accumulation of inflammatory cells within the crypts of the intestine),
- depletion of the mucin layer in the intestine,
- surface integrity,
- chronic inflammatory cell infiltration, and
- Crypt irregularities in the colon.
Finally, they assessed the relationship between the levels of immune cell biomarkers, tissue healing, and long-term outcomes, including symptomatic recurrence after standard therapy.
Their results suggested that after the 18-month follow-up, a higher proportion of CD177-positive neutrophils, CD40L-positive T cells, and eosinophils were highly predictive of disease recurrence. Notably, patients who achieved histological healing had a lower proportion of inflammatory immune cells, compared to those who did not achieve healing.
Inflammatory Cell Enumeration Index (ICEI)
Next, based on the threshold values of colonic CD177-positive neutrophils, eosinophils, and CD40L-positive T cells from healthy donors, the researchers developed a measure called the ‘inflammatory cell enumeration index (ICEI).’ Patients with lower values than the established ICEI threshold, and without crypt abscesses, mucin depletion, surface epithelial damage, and crypt architectural irregularities, were considered as having achieved tissue healing.
Furthermore, they found that ICEI could reliably stratify patients based on those with healed tissue and those with active tissue. Notably, only 13.1% of patients from the healed group experienced a recurrence compared to 40.7% of patients from the group with active tissue.
Further, ICEI combined with other established indices provided a more accurate prediction of histological healing and recurrence than either score alone. While currently, a standard and uniform format for grading mucosal inflammation is lacking, the proposed ICEI could serve as a good choice for predicting the prognosis of patients with UC.
This can, in turn, help reduce overtreatment in clinical practice by helping in the evaluation of MH and identification of high-risk patients following clinical healing. Overall, these findings pave the way for the development of accurate prediction models for assessing the risk of recurrence in patients with UC.
Sharing his concluding thoughts on the clinical applications of their work, Prof. Liu says, “As clinical therapy goals in UC continue to evolve, from endoscopic MH to histopathological healing, the ICEI offers a valuable tool for assessing and predicting the prognosis of UC patients. These advancements will contribute to a deeper understanding of UC and offer opportunities for more tailored and effective management strategies.”
Reference:
- Augmented Development and validation of a novel criterion of histologic healing in ulcerative colitis defined by inflammatory cell enumeration in lamina propria mucosae: A multicenter retrospective cohort in China – ( https:doi.org/10.1097/CM9.0000000000003154)
Source-Eurekalert