- Neuromodulation alters nerve activity to manage Overactive bladder symptoms effectively
- Techniques include sacral neuromodulation, posterior tibial nerve stimulation, and pudendal nerve stimulation
- Patient selection and ongoing management are crucial for optimizing treatment outcomes
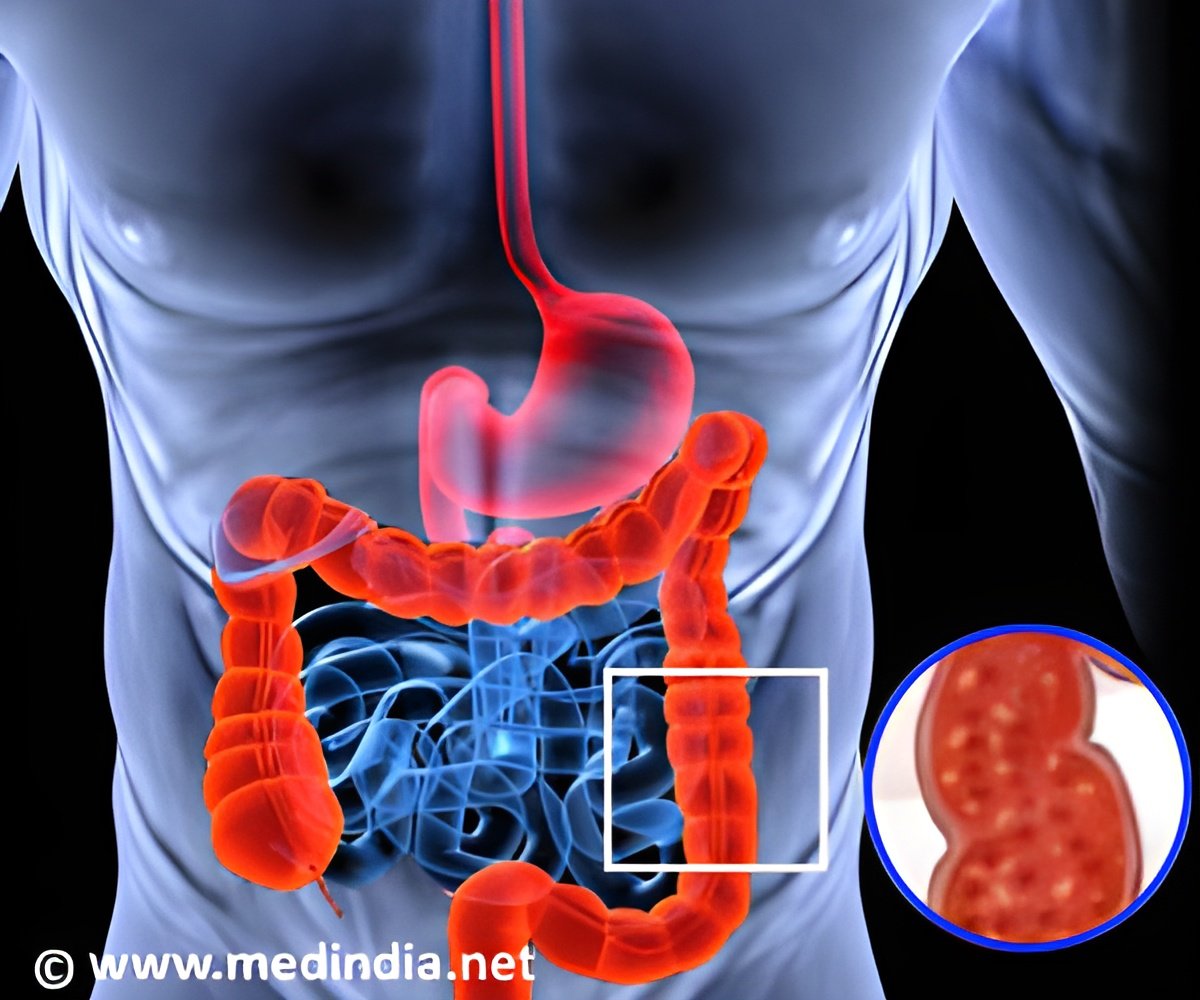
Overactive bladder (OAB) is a prevalent condition affecting millions globally, characterized by symptoms such as urgency, frequent urination, and nocturia. Despite various treatment options, many patients experience inadequate relief or intolerable side effects from first-line therapies (1✔ ✔Trusted Source
Neuromodulation for overactive bladder
).
Neuromodulation has emerged as a promising alternative, offering a minimally invasive, reversible treatment option for those unresponsive to conventional treatments. This article provides a comprehensive overview of neuromodulation for OAB, its mechanisms, techniques, and clinical significance.
Initial management of OAB generally involves behavioral modifications, pharmacotherapy, and physical therapy, which may be used alone or in combination.
Neuromodulation as a Treatment for Overactive bladder
Neuromodulation offers a novel approach to managing Overactive bladder by targeting the nervous system’s ability to regulate bladder function. This treatment method involves modulating nerve activity to improve symptoms of OAB. It has gained prominence due to its minimally invasive nature, reversibility, and overall effectiveness.
Mechanism of Action: Neuromodulation is thought to alleviate OAB symptoms by altering somatic afferent sensory processing in the sacral spinal cord. By modulating nerve signals, neuromodulation can influence the bladder’s overactivity and improve patient outcomes.
Types of Neuromodulation Techniques
1. Sacral Neuromodulation (SNM)
- Sacral neuromodulation is the most established neuromodulation technique for OAB. It targets the S3 nerve root, which plays a crucial role in bladder control.
- An implanted device sends electrical impulses to the S3 nerve root, modulating its activity and thus affecting bladder function.
- Sacral neuromodulation has a robust body of evidence supporting its safety and efficacy. Long-term studies demonstrate significant improvements in OAB symptoms and quality of life.
2. Posterior Tibial Nerve Stimulation (PTNS)
- PTNS involves stimulating the tibial nerve, which indirectly influences bladder function through its connections with the sacral plexus.
- A thin needle electrode is inserted near the tibial nerve in the ankle, delivering electrical impulses to modulate nerve activity.
- Research shows positive outcomes with PTNS for OAB, though it is less established compared to sacral neuromodulation.
3. Pudendal Nerve Stimulation (PNS)
- PNS targets the pudendal nerve, which also interacts with the sacral spinal cord to affect bladder control.
- A stimulating electrode is placed near the pudendal nerve to deliver electrical impulses.
- Although promising, PNS is less commonly used and studied compared to SNM and PTNS. Ongoing research continues to refine its role in OAB management.
Comparison of Neuromodulation Techniques
Each neuromodulation technique has specific indications, procedural differences, and clinical outcomes:
Sacral Neuromodulation: Preferred for its extensive evidence base and long-term safety. It is the primary target for OAB treatment.
Advertisement
Posterior Tibial Nerve Stimulation: Useful for patients who prefer a less invasive approach with a lower risk of complications.
Pudendal Nerve Stimulation: Still evolving, with studies needed to fully establish its role and efficacy in treating OAB.
Advertisement
Patient Selection and Management of Overactive Bladder
Patient selection is critical for optimizing treatment outcomes. Factors to consider include:
Severity and Duration of Symptoms: Patients with refractory OAB symptoms may benefit more from neuromodulation.
Previous Treatments: Patients who have failed conservative therapies are ideal candidates for neuromodulation.
Patient Preferences: Individual preferences regarding invasiveness and treatment reversibility play a role in choosing the appropriate technique.
Postoperative management and follow-up are essential for ensuring treatment efficacy and addressing any complications. Regular assessments help in adjusting therapy and ensuring sustained improvements.
Neuromodulation has revolutionized the management of Overactive bladder by offering a viable option for patients who do not respond to first-line treatments. With its minimally invasive nature, positive outcomes, and reversibility, it stands out as an attractive treatment modality. Sacral neuromodulation remains the most established technique, while posterior tibial and pudendal nerve stimulation offer additional alternatives. Urologists should be proficient in these techniques, understanding their indications, procedural nuances, and patient management strategies to optimize treatment outcomes for OAB.
By progressing from least to most invasive treatments, neuromodulation provides a valuable approach in the continuum of OAB management, enhancing patient quality of life and offering hope where traditional therapies fall short.
Reference:
- Neuromodulation for overactive bladder – (https://www.nature.com/articles/nrurol.2013.143)
Source-Medindia