“Not only was survival better than after biological or mechanical aortic valve replacement, but it was also identical to the matched U.S. general population. To this day, this is the only operation that has ever been shown to restore survival after aortic valve replacement in young adults,” says lead author Ismail El-Hamamsy, MD, Ph.D., Mount Sinai Randall B. Griepp, MD Professor of Cardiovascular Surgery at the Icahn School of Medicine at Mount Sinai and Director of Aortic Surgery for the Mount Sinai Health System.
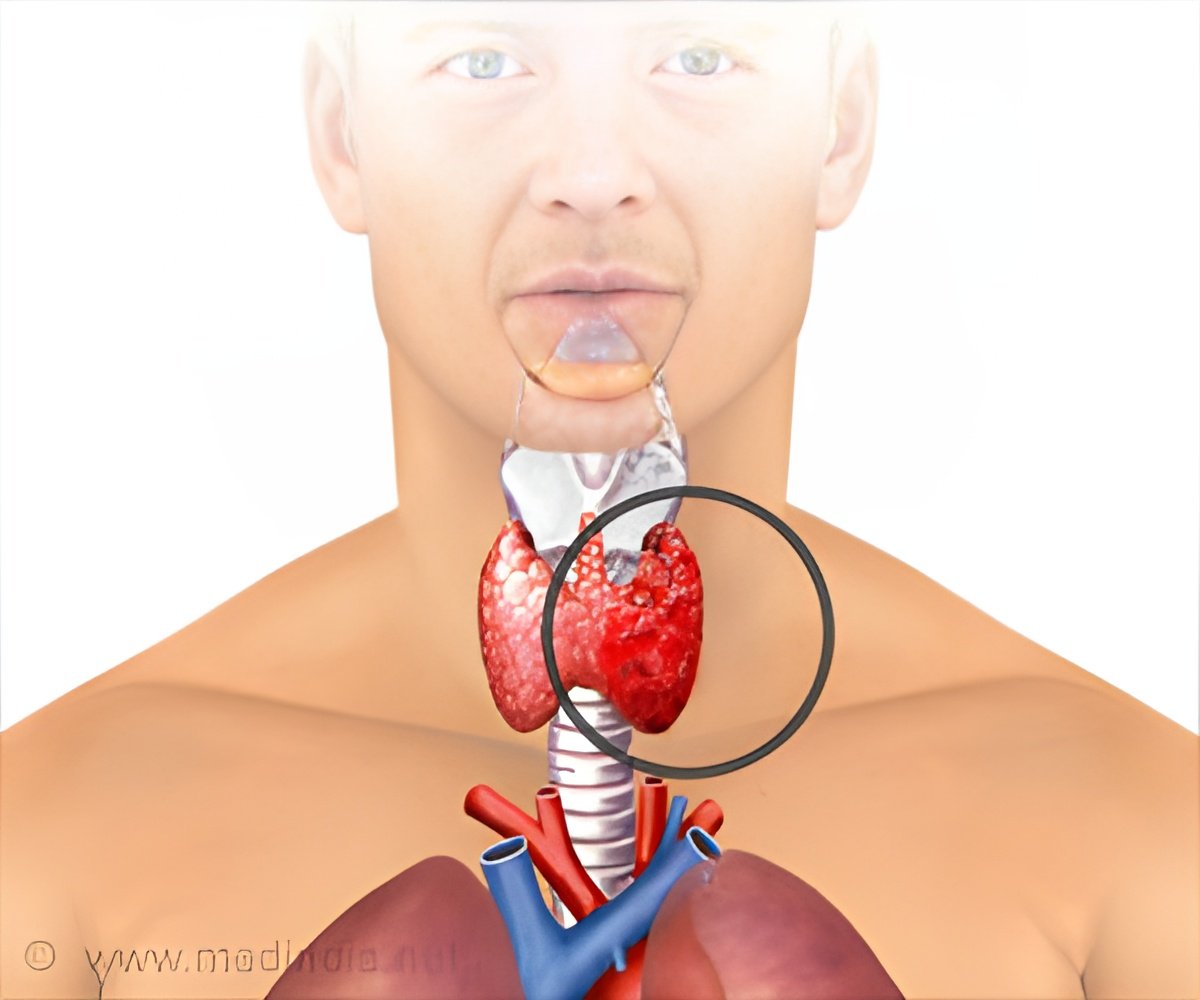
The aortic valve controls blood flow from the heart into the aorta, the main artery that feeds blood to most of the body. When the valve doesn’t work correctly, patients may need a replacement to preserve the function of the heart muscle and prevent issues such as heart failure or sudden cardiac death.
The standard open-heart procedures for repair include mechanical valve replacement, which uses a manufactured valve that requires patients to take life-long blood thinners to prevent stroke, as well as make some lifestyle modifications or a biological aortic valve replacement from a human or animal donor, which may last up to 20 years that requires earlier reoperation in younger patients than a mechanical valve.
The Ross procedure is a more complex operation where a surgeon replaces the diseased aortic valve with the patient’s living pulmonary valve, which is a mirror image of a normal aortic valve.
This is the fundamental difference between the Ross procedure and a biological or mechanical valve replacement, which is a critical factor for successful long-term outcomes in patients.
Researchers analyzed records of 1,302 patients between 18 and 50 years old who underwent first-time elective aortic valve replacement surgery in California and New York State between January 1, 1997, and December 31, 2014.
Patients were equally divided into three categories using propensity-matched analysis to eliminate any baseline differences; one-third of them had the Ross procedure, one-third had a biological valve replacement, and the rest had a mechanical valve replacement.
The retrospective study compared the long-term survival and risk of valve-related complications (including stroke, major bleeding, reoperation, and acute endocarditis) according to the surgical procedure.
Investigators looked at outcomes 15 years post-procedure and found that patient survival was significantly better after the Ross procedure. At 15 years, overall mortality was more than twofold higher if the patients received a biological or mechanical aortic valve versus a Ross procedure.
Furthermore, survival after the Ross procedure (93 percent survival at 15 years) was identical when compared to people of the same age and sex in the U.S. general population who did not have aortic valve replacement surgery.
In terms of valve-related complications, the Ross procedure was associated with a significantly lower risk of stroke or major bleeding than a mechanical valve (3.8 percent after a Ross procedure versus 13 percent after a mechanical valve at 15 years).
Similarly, the Ross procedure was associated with significantly fewer reoperations (17 percent versus 30 percent at 15 years) and endocarditisan infection of the heart tissuethan a biological valve (2.3 percent versus 8.5 percent at 15 years). At 15 years, however, the risk of reoperation was higher after a Ross procedure than after mechanical valve replacement (17 percent versus 7.4 percent at 15 years).
The study also looked at 30-day mortality after the occurrence of any valve-related complication, including stroke, major bleeding, endocarditis, or reoperation.
Researchers found the lowest mortality was linked to reoperation (1 percent), whereas if patients had a stroke, major bleeding, or endocarditis, the associated mortality was at least three times higher (5.6 percent after a stroke and 13.5 percent after endocarditis).
Researchers hope that this will further encourage the development of regional Ross centers of excellence to improve patient access and safety.
Furthermore, they are also are working on improving the durability of the Ross procedure so that even fewer patients ever need a reoperation.
Source: Medindia