It affects children of all ages but is more common in older children and teenagers. The disorder generally occurs 2-6 weeks after infection with the SARS-CoV-2 virus.
Symptoms include persistent high fever, often accompanied by abdominal pain, vomiting, red eyes and red rash. Severely affected children have developed heart inflammation, with shock and failure of multiple organs.
With proper treatment the majority of affected children have recovered well. However, worldwide most reports suggest a fatality rate of 2-4%.
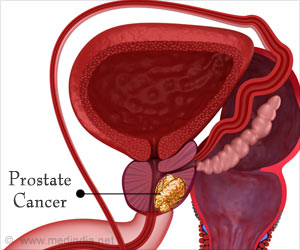
Coronary arteries may get widened. This is also known to happen in another condition called Kawasaki disease. Researchers investigated two initial treatments: Methyl prednisolone and Immunoglobulin.
The study involved doctors uploading information about patient outcomes onto an online database, and was not a randomised controlled trial.
All three treatments (immunoglobulin, immunoglobulin combined with corticosteroids and cortico-steroids alone) resulted in more rapid resolution of inflammation, as measured by the level of a protein that indicates inflammation levels in the body, called C-reactive protein (CRP).
The CRP fell by half approximately one day quicker in those receiving treatment. There were no clear differences between the three treatments in rate of recovery from organ failure, or progression to organ failure.
The number of fatal cases (2%) was too low to enable comparison between treatments, but death was included in a combined assessment with organ failure, which found no significant differences between the three treatments.
There was evidence of a lower rate of organ support or death at 2 days in those receiving steroids alone as initial treatment, compared to immunoglobulin alone.
Dr Elizabeth Whittaker, one of the authors of the study from Imperial’s Department of Infectious Disease, and one of the first doctors in the world to originally identify this condition, together with colleagues at Imperial College and Imperial College Healthcare NHS Trust, said: “The finding that outcome is similar for patients treated with steroids alone as with those treated with steroids and immunoglobulin or immunoglobulin alone, suggests that steroids may be a cheaper and more available alternative to immunoglobulin.
Corticosteroids are cheap and available worldwide whereas immunoglobulin is expensive, and there is a worldwide shortage of it. This is a particular problem in many low and middle income countries. “
However the authors stress there is insufficient data to establish that all three treatments are equivalent in preventing coronary artery aneurysms. Around 6 per cent of children in the study suffered a coronary artery aneurysm.
Professor Michael Levin, from the Department of Infectious Disease at Imperial, who led the study, said: “The study has been a real example of international collaboration and the willingness of paediatricians in many countries to share their data and experience to enable important questions as to optimal treatment to be answered.
Treatments with immunoglobulin, steroids or a combination of both agents all result in more rapid resolution of inflammation (and have similar rates of progression to organ failure or recovery from critical illness), will be of great value to paediatricians worldwide in their treatment of children with this new disorder.
Immunoglobulin is unavailable or in short supply in many countries, and is expensive. The findings of this study may provide some reassurance for those who only have access to corticosteroids, particularly in those countries with more limited resources.
Our study does not yet provide a definitive answer as to whether any of the treatments lowers the risk of coronary artery aneurysms, as the numbers with this complication were too low. The study is continuing to enrol patients and our planned further analysis with larger numbers of patients should provide answers to this question.”
Source: Medindia