Genetic mapping of atherosclerotic plaque cells can predict future heart health.

Genetic traits shape the cellular makeup of atherosclerotic plaques, ultimately influencing their potential to trigger strokes or heart attacks over time, suggest a new study led by a team of researchers at Karolinska Institutet. This new understanding could enhance future risk assessment and treatment strategies for patients with atherosclerosis.
The findings of the study are published in the European Heart Journal (1✔ ✔Trusted Source
Atheroma transcriptomics identifies ARNTL as a smooth muscle cell regulator and with clinical and genetic data improves risk stratification
).
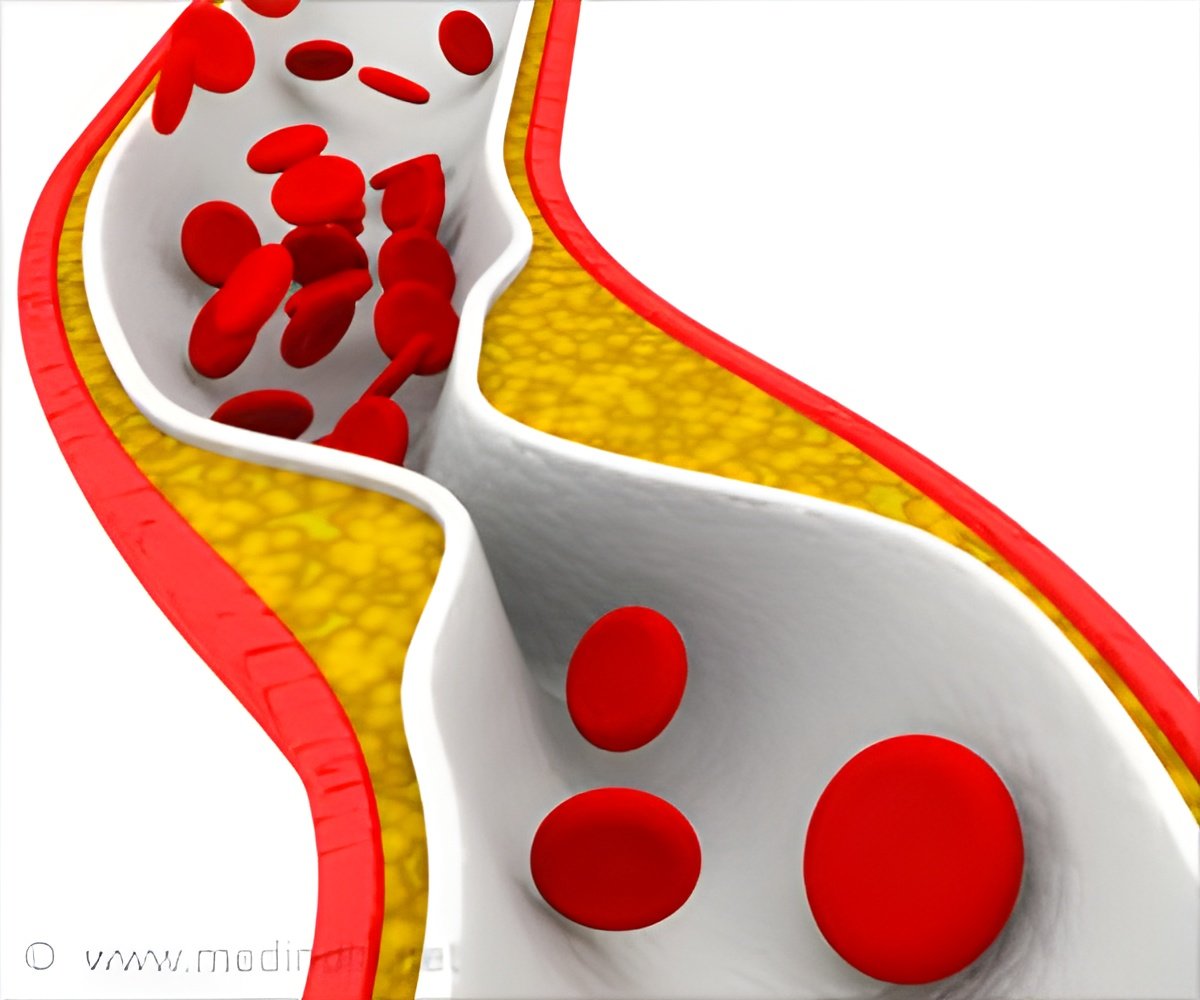
Atherosclerosis: The Hidden Danger to Your Heart
Atherosclerosis is the main cause of cardiovascular diseases such as stroke and heart attack. Researchers at Karolinska Institutet in Sweden, together with colleagues at the universities of Stanford and Virginia in the USA, have now succeeded in mapping the association between genetic factors and the composition of different cell types in atherosclerotic plaques. The research was based on analyses of tissue samples from patients with atherosclerosis stored in a biobank (Biobank of Karolinska Endarterectomies, BiKE).
Legacy of Plaque: Understanding the Genetic Roots of Atherosclerosis
“Previous research has shown that heredity is important for the levels of cholesterol, other lipids and circulating immune cells in the blood, but now we see that heredity also affects the composition of smooth muscle cells in the blood vessels of atherosclerotic patients,” says Ljubica Matic, docent at the Department of Molecular Medicine and Surgery at Karolinska Institutet who led the study. “This can affect the development of atherosclerotic plaques, but also the tendency for the plaques to become unstable and cause a stroke.”
Using this data on heredity, the researchers have been able to categorize patients into three different groups.
“The first group are those with the most severe profile and in our material they have usually already had a stroke,” says Ljubica Matic. “For patients at lower risk, the vessels have formed plaques but without causing a stroke. The third group of patients is somewhere in between these two and often have kidney disease in combination with atherosclerosis. We also have preliminary evidence that the same concept may be valid in heart attacks.”
The new knowledge about genetic influence on plaque cells can be used together with modern diagnostic imaging and AI to make better assessments of future risk of stroke or heart attack, or prediction of response to different drugs.
“We have done similar integrative studies for smaller cohorts of patients in other previously published papers to prove that it works, but of course the concept needs to be tested on a larger scale before it can be introduced into clinical practice,” says Professor Ulf Hedin at the same department at Karolinska Institutet. “We will be working intensively on these modern, so called multi-modal studies in the future, through our new EU Horizon 2020 NextGen and MedTechLabs funded projects”.
Fatty Layers of Danger: Plaque Formation in Atherosclerosis
Atherosclerotic plaques form over decades through the deposition of blood lipids such as cholesterol in the innermost layer of the vessel wall. As the plaques become unstable and rupture, blood clots form and can completely block the vessel or be carried by the bloodstream to other organs such as the brain. In either case, there is a lack of oxygen in the tissues as the blood does not reach them, which can cause a heart attack or a stroke.
Although mortality from cardiovascular disease has steadily declined over the last 50 years due to better understanding of the mechanisms, better preventive treatments and diagnostics and, not least, better diet and exercise habits, it is still the leading cause of death in Sweden.
The research was funded by, among others, the Swedish Research Council, the Swedish Heart-Lung Foundation and Karolinska Institutet. Clint L. Miller has received support from Astra Zeneca for an unrelated project. The other authors declare no conflicts of interest.
References:
- Atheroma transcriptomics identifies ARNTL as a smooth muscle cell regulator and with clinical and genetic data improves risk stratification – (https://academic.oup.com/eurheartj/advance-
article/doi/10.1093/eurheartj/ehae768/7903013)
Source-Eurekalert